Xerostomia, also commonly known as dry mouth, is a condition characterized by a persistent decrease in saliva production. Saliva plays a vital role in oral health, aiding in digestion, lubrication, taste perception, and keeping the mouth clean. When saliva production is compromised, it can lead to a range of uncomfortable and potentially harmful consequences.
What is Xerostomia?
Saliva is a complex fluid produced by glands in the mouth. It contains enzymes that break down food, electrolytes to maintain hydration, and antibacterial properties to fight germs. In xerostomia, the salivary glands either don’t produce enough saliva or produce saliva with an altered composition. This can lead to a feeling of dryness, irritation, and discomfort in the mouth.
There are two main types of xerostomia:
- Primary xerostomia: This is a less common form where the salivary glands themselves are damaged or diseased. This can be caused by autoimmune diseases like Sjogren’s syndrome, sarcoidosis, or certain medications.
- Secondary xerostomia: This is the more prevalent form and occurs when something else disrupts saliva production. Examples include certain medications, dehydration, radiation therapy to the head and neck, and some medical conditions like diabetes.
5 Symptoms of Xerostomia
The most common symptom of xerostomia is a dry, parched feeling in the mouth. This dryness can be constant or come and go throughout the day. Other symptoms associated with xerostomia can include:
- Difficulty swallowing: Reduced saliva makes it harder to moisten and form a bolus (a ball of food) for swallowing, leading to discomfort and potentially choking hazards.
- Difficulty speaking: Dryness can affect the tongue’s ability to move freely, making speech raspy or difficult to understand.
- Altered taste perception: Saliva plays a role in carrying taste bud signals to the brain. When saliva production is low, taste can become dull or distorted.
- Increased risk of cavities: Saliva naturally washes away food particles and neutralizes acids in the mouth, helping to prevent tooth decay. Reduced saliva flow can lead to a buildup of plaque and an increased risk of cavities.
- Mouth sores and burning sensation: Dryness can irritate the tissues in the mouth, leading to discomfort and soreness.
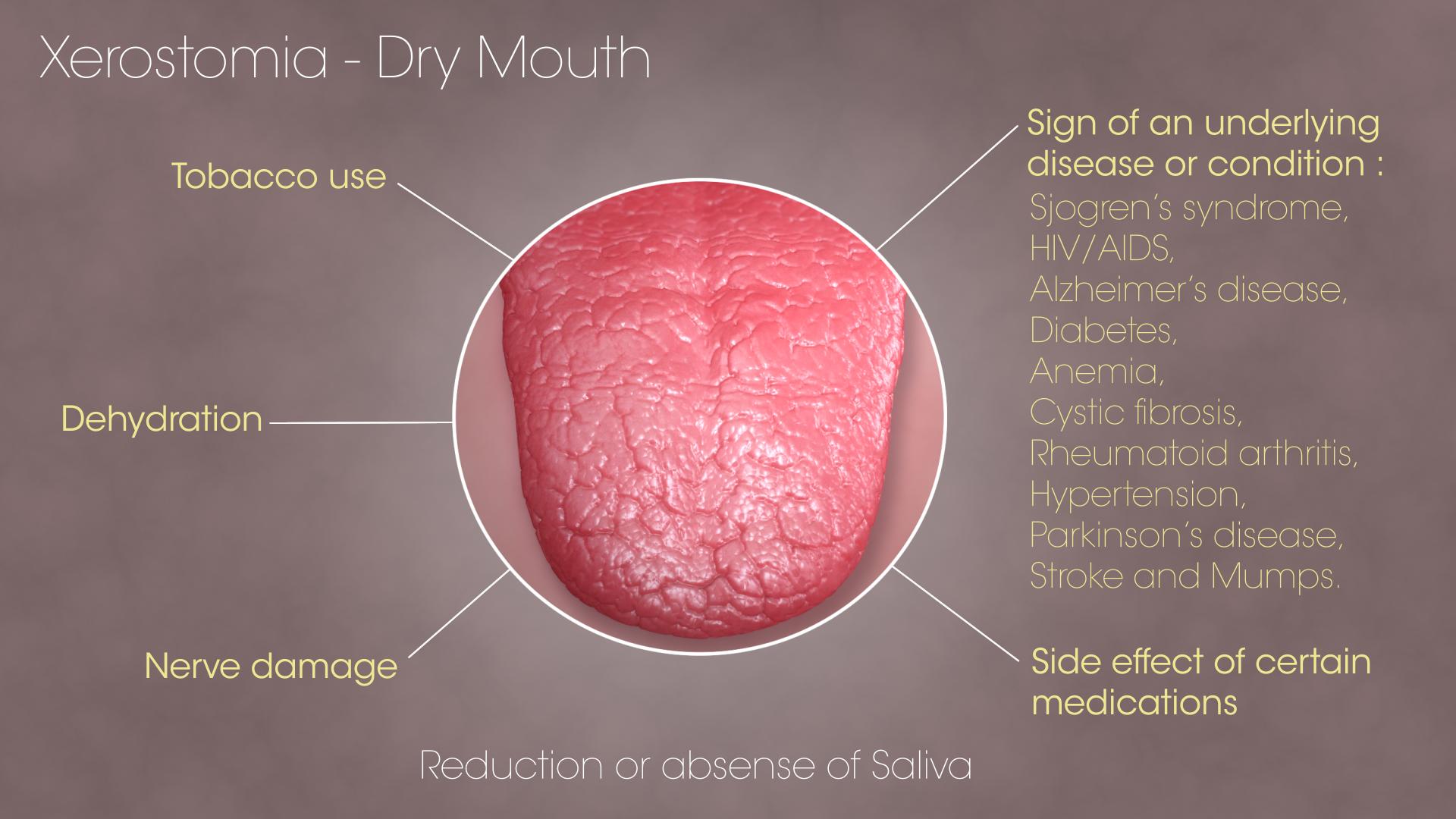
5 Causes of Xerostomia
Several factors can contribute to xerostomia. Here are five common causes:
- Medications: Many medications can have dry mouth as a side effect. These include antihistamines, antidepressants, decongestants, diuretics, and some blood pressure medications.
- Dehydration: Not drinking enough fluids can lead to overall dehydration, including dryness in the mouth.
- Medical conditions: Certain medical conditions like diabetes, Sjogren’s syndrome, and HIV/AIDS can affect salivary gland function and lead to xerostomia.
- Age: Saliva production can naturally decrease with age, making older adults more susceptible to xerostomia.
- Smoking and tobacco use: Smoking and tobacco use can irritate the mouth and salivary glands, contributing to xerostomia.
How to Manage Xerostomia
While there isn’t a complete cure for xerostomia, there are ways to manage the symptoms and improve oral comfort. Here are some tips:
- Stay hydrated: Drinking plenty of water throughout the day is crucial to keep the mouth moist. Aim for eight glasses of water per day or more depending on your activity level and climate.
- Sugar-free lozenges and gum: Sucking on sugar-free lozenges or chewing sugar-free gum can stimulate saliva production and keep the mouth moist.
- Artificial saliva products: These over-the-counter sprays or gels can provide temporary relief from dryness.
- Moisturizers for lips: Using lip balms or ointments can help prevent dryness and cracking of the lips.
- Reduce consumption of drying substances: Limit caffeine and alcohol, which can further dehydrate the mouth.
- Maintain good oral hygiene: Brush twice a day and floss daily to remove plaque and prevent cavities, which are more likely to occur with reduced saliva flow.
- Talk to your doctor about medications: If you suspect a medication is causing dry mouth, discuss alternative options with your doctor.
- Consider using a humidifier: Adding moisture to the air, especially at night, can help alleviate dryness in the mouth.
FAQs
Is Xerostomia Harmful?
Yes, xerostomia can be harmful if left unmanaged. Here’s why:
- Increased risk of cavities: As discussed earlier, reduced saliva flow disrupts the mouth’s natural defenses against tooth decay. This can lead to a rapid buildup of plaque and a higher risk of cavities.
- Fungal infections: A dry mouth environment creates a breeding ground for fungal infections, particularly Candida albicans, which can cause thrush. This condition manifests as white patches on the tongue and inner cheeks, accompanied by burning and discomfort.
- Gum disease: Dryness can contribute to gum inflammation (gingivitis) and potentially progress to gum disease (periodontitis) if left untreated.
- Nutritional deficiencies: Difficulty swallowing and altered taste perception can lead to changes in eating habits and potentially contribute to nutritional deficiencies.
- Social and emotional impact: Dry mouth can negatively impact social interactions due to difficulty speaking and bad breath. Additionally, the discomfort and pain associated with xerostomia can affect emotional well-being and quality of life.
Conclusion
Xerostomia, while not a life-threatening condition, can significantly impact oral health and overall well-being. However, with proper management strategies and potential adjustments in medication or lifestyle habits, individuals with xerostomia can experience significant relief from symptoms and maintain good oral health. If you suspect you have xerostomia, it’s crucial to consult with your doctor or dentist in Baulkham hills to determine the underlying cause and develop a personalized management plan.